Prevention of Fetal Alcohol Spectrum Disorders
R. Louise Floyd, RN, DSN, Clark Denny, PhD, Mary Kate Weber, MPH
Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, USA
Introduction
The scientific literature addressing alcohol use during pregnancy and the wide range of associated consequences has grown immensely over time in breadth, scope and understanding since the first article on Fetal Alcohol Syndrome (FAS) in the U.S. appeared in a 1973 edition of The Lancet.1 In 1996, the Institute of Medicine (IOM) released a congressionally-mandated report by the Committee to Study Fetal Alcohol Syndrome that reviewed and summarized the knowledge amassed up to the mid-1990s. This seminal report provided recommendations concerning the diagnosis, epidemiology, prevention and treatment of FAS.2 The committee recommended that the birth defects and developmental disabilities attributed to prenatal alcohol exposure be grouped into the four categories: Fetal Alcohol Syndrome (FAS), Partial Fetal Alcohol Syndrome (P-FAS), Alcohol-Related Neurodevelopment Disorder (ARND); and Alcohol-Related Birth Defects and Developmental Disorders (ARBD). In 2004, the term Fetal Alcohol Spectrum Disorders (FASD) was adopted as an umbrella term describing the wide range of physical, mental, behavioural and learning disabilities that can result from alcohol use during pregnancy, encompassing the four conditions listed above.3 The most studied condition of the spectrum is Fetal Alcohol Syndrome. Current estimates of the prevalence of FAS in the U.S. range from 0.2 to 1.5 per 1,000 live births to 2 per 1,000 live births.4,5,6 Prevalence rates of the full spectrum are generally thought to be three times the rate of FAS alone.7 Estimates of the lifetime cost of FAS have been reported at $2 million per case.8 Current efforts are underway among federal agencies, universities and professional societies to find a successful roadmap for combating this preventable, public health problem that affects America’s children, families and society. This chapter will provide a brief overview of the problem, its challenges, and potential prevention solutions.
Subject
Survey results from the Centers for Disease Control and Prevention (CDC) using the Behavioral Risk Factor Surveillance System (BRFSS) report long-term trends in high rates of alcohol use among women of childbearing age (18-44) in the U.S. Between 1991 and 2005, approximately 55% of non-pregnant, and 11% of pregnant women, reported alcohol use in the past month.9 Of special concern is that among those reporting alcohol use, 13% of non-pregnant and 2% of pregnant women reported binge drinking (defined as five or more drinks on one occasion in the referenced data set). Another study reported that binge drinking episodes increased from 1993-2001 with an estimated average of 37 episodes for each woman of childbearing age who reported binge drinking in 2001.10 Binge drinking rates continued to rise from 11.9% in 2001 to 12.4% in 2002, and 13.0% in 2003. Women who reported binges, reported an average of three episodes per month. The highest binge rates were among women 18-24 years of age.11
In 2004, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended a new definition of “binge drinking” for women – an episode of four or more alcoholic drinks consumed in a two-hour period.12
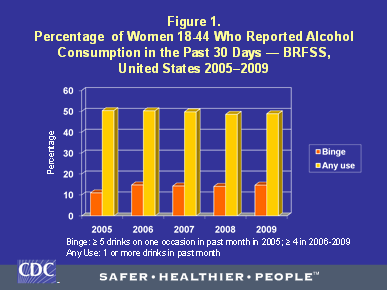
Figure 1 shows the prevalence of any alcohol consumption and binge drinking in the past 30 days between 2005 and 2009 in women aged 18-44 in the U.S. The graph includes data prior to and after the BRFSS adopted the new NIAAA definition of binge drinking for women. As shown, the prevalence of any reported drinking varied little and stayed around 50 percent for all five years. As would be expected, the prevalence of binge drinking increased from 11.0% in 2005 to 14.8% in 2006 when the definition of binge drinking changed from ≥ 5 drinks on an occasion to ≥ 4 drinks on an occasion. This suggests that surveys still using the 5-drink definition of a binge for both males and females may potentially underestimate the scope of risky drinking in women. From 2006 to 2009, the prevalence of binge drinking varied slightly between 14 and 15%. The data for the table are from respondents to the BRFSS who lived in the 50 states and the District of Columbia. These levels of any alcohol use in the past month, especially binge drinking, represent a significant risk because approximately half of all pregnancies in the U.S. are unplanned.13 Further, many women do not realize that they are pregnant in the beginning of their pregnancies and may continue drinking during the early weeks of gestation.
Studies find marked differences in rates of alcohol consumption among non-pregnant women of childbearing age and pregnant women because most women reduce alcohol use when they find they are pregnant.14,15 One Danish study found that the rate of reported binge drinking during pregnancy peaked at week three and thereafter continued to decline until week seven, after which binge drinking was rarely reported.16 A Canadian study found that women in the preconception period did not change their drinking amounts and patterns while they were trying to become pregnant but after pregnancy confirmation, quantity, frequency and binge drinking declined significantly. The authors concluded that more preconception counseling should focus on risks of alcohol use during periods when pregnancy can occur (sexual activity and no use of contraception).17
Problems
While progress has been made in the prevention arena, it appears that women are not always hearing consistent messages about alcohol use during pregnancy. For example, in one study, women reported that they receive conflicting messages about alcohol use during pregnancy from family, friends, and providers, especially about what type of alcohol to drink and how much is dangerous.18 As stated earlier, prenatal alcohol exposure is a common occurrence in the U.S. with 1 in 8 pregnant women self-reporting alcohol use during pregnancy.9 This behaviour, while modifiable, continues to persist despite the advisories and recommendations of experts calling for women who are pregnant, planning a pregnancy or could become pregnant to abstain from alcohol use. These include the 2005 reissue of the Surgeon General’s Advisory on Alcohol Use in Pregnancy,19 the Department of Health and Human Services’ Dietary Guidelines for Americans,20 the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics21 and the National Institute on Alcohol Abuse and Alcoholism (A Clinician’s Guide).22 While there is a significant reduction in alcohol use after pregnancy recognition occurs overall, there is evidence that many women continue to drink while trying to get pregnant and after pregnancy recognition. In one study, based on a national sample of women of childbearing age, 45% of women reported drinking in the three months prior to pregnancy recognition, and 60% of women who reported drinking also reported not learning they were pregnant until four to six weeks gestation.23 In another study, 50% of women who were trying to conceive reported continuing to drink alcohol.17
Research Context
The 1996 IOM report proposed an IOM Model for FAS Prevention that recommended three levels of prevention to reduce Fetal Alcohol Syndrome: Universal Prevention of Maternal Alcohol Abuse; Selective Prevention of Maternal Alcohol Abuse; and Indicated Prevention of FAS.
- Universal Prevention focuses on creating high levels of awareness of the consequences of alcohol use during pregnancy among the general population and women in particular. Examples include media campaigns, alcohol bottle labeling and national advisories.
- Selective Prevention strategies are directed toward sub-groups of the population known to be at increased risk for having an alcohol-exposed pregnancy (AEP). Examples include targeted screening and brief interventions tailored to the specific sub-group.
- Indicated Prevention includes multiple strategies of case identification of maternal alcohol abuse, brief intervention, formal treatment, long-term treatment and aftercare. Research has addressed many of the strategies used in the proposed three levels of prevention and found that alcohol screening and brief interventions (SBI) or extended brief interventions provide the most consistent evidence for success in bringing about alcohol use reductions. Systematic reviews by the United States Preventive Services Task Force (USPSTF) on alcohol screening and brief interventions concluded that they should be used in adults with alcohol use problems in primary care settings including non-pregnant and pregnant childbearing aged women. While acknowledging the limited number of studies on SBI for non-pregnant and pregnant women, they concluded that the benefits of SBI to reduce alcohol misuse outweighed any potential harms.24 Recent studies of effective alcohol screening and brief interventions among pregnant and preconceptional women have been reported since the USPSTF recommendations were issued.25,26,27 Many employ previously developed brief screening instruments such as the T-ACE, TWEAK, AUDIT, and more recently, the AUDIT-C. A fuller description of studies related to the three levels of prevention is provided in Reducing Alcohol-Exposed Pregnancies: A Report of the National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect.28 However, a 2009 systematic review by the Cochrane Collaboration on interventions aimed at reducing alcohol consumption in pregnant women and women planning pregnancy found only four studies that met their standards for inclusion within the years targeted in the search (1966-2007). They concluded that small sample sizes, methodological differences, inconsistency in findings, and other issues made it difficult to determine the basis for evidence-based recommendations. The review further called for additional well designed studies in this population.29
Key Research Questions and Research Gaps
Addressing important health problems, such as FAS, that can impair the health of individuals across their lifespan requires a substantive understanding of the problem and why we should be concerned about it, its associated risk factors, the health and economic impact, and importantly, what can be done about it. While there is consensus on the salient manifestations of FAS, estimates for how many children are affected with this syndrome varies widely as mentioned earlier.6 Efficient population-based surveillance systems need to be developed to provide information on the full impact of prenatal alcohol exposure providing information for action and to build the public will and support necessary to prevent FASDs. Recent formative work in this area suggests that misconceptions about drinking during pregnancy continue to exist and women are not receiving clear and consistent messages about alcohol use before and during pregnancy. Efforts are needed to better frame messaging around drinking during pregnancy within the current climate of mixed messages that women sometimes receive from health providers, friends and family, and through the media.30 Further research is also needed to better increase our understanding of women’s knowledge, attitudes and opinions about alcohol use and pregnancy and the role alcohol plays in the lives of women of reproductive age. This information can help inform development of risk communication messages about the consequences of alcohol use during pregnancy, with appropriate content and tone for diverse populations of women. Also, despite the concerning rates of alcohol use among women of childbearing age, screening for alcohol use among female patients is not universally part of the standard of care among health providers. Ongoing provider education and training about FASDs and the risks associated with alcohol use and pregnancy are an important component of FASD prevention activities. In order to build a stronger evidence base for what works best in preventing alcohol-exposed pregnancy, more intervention research is needed to address the effectiveness of screening and brief interventions and other prevention strategies in women who could become pregnant, planning a pregnancy, or are currently pregnant.
The 2005 Message to Women from the U.S. Surgeon General Advisory advised women who are pregnant or considering pregnancy to abstain from alcohol use. Concern has arisen about this advisory among providers and women who only drink occasionally and chose to continue light to moderate alcohol use during pregnancy. Unfortunately, the evidence base for answering the question of the impact of light to moderate alcohol use on the exposed fetus includes studies with mixed results and contradictory findings. Clearly more in-depth research is needed to more definitively address the question of safety of light to moderate alcohol use during pregnancy.
Trends in alcohol use among women of childbearing age have remained steady suggesting that current prevention messages may not be reaching those to whom they are most relevant, may not be deemed credible, or are competing with conflicting or inaccurate messages from other sources (e.g., the media, health providers, and some internet sources). A consensus based on a thorough review of the scientific evidence could do much to establish consistency in advice and practice strategies to help women avoid alcohol-exposed pregnancies that could lead to FASDs.
Conclusions
Our understanding of the biomedical, epidemiological, and public health prevention strategies for FASD has grown exponentially over the past 38 years.31 Despite progress made in knowledge, women of reproductive age (pregnant and non-pregnant) continue to report current alcohol consumption levels similar to those of 1991. The primary challenges at this point in time are to fill in the gaps preventing us from taking knowledge gained to the front line health providers and convince the public of the threat posed by risky drinking for women of reproductive age in general, and risks posed to the fetus if they are pregnant or could become pregnant. Of key importance is teaching health providers in primary care settings how to screen and provide brief interventions and referral to women who are at risk for alcohol-exposed pregnancies.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Jones KL, Smith DW, Ulleland CN, Streissguth AP. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267-1271.
- Stratton KR, Howe C, Battaglia F. editors. Fetal alcohol syndrome: Diagnosis, epidemiology, prevention , and treatment. Washington, DC: National Academy Press; 1996.
- Bertrand J, Floyd RL, Weber MK, O’Connor M, Riley EP, Johnson KA, Cohen DE, National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect. Guidelines for referral and diagnosis. Atlanta, GA: Centers for Disease Control and prevention; 2004.
- CDC. Fetal alcohol syndrome—Alaska, Arizona, Colorado, and New York, 1995-1997. MMWR. 2002;51:433-435.
- CDC. Surveillance for fetal alcohol syndrome using multiple sources – Atlanta, Georgia, 1981-1989. MMWR. 1997;46:1118—20.
- May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome: a summary. Alcohol Res Health. 2001;159-167.
- Sampson PD, Streissguth AP, Bookstein FL, Little RE, Clarren SK, Dehaene P, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56(5):317-26.
- Lupton C, Burd L, Harwood R. Cost of fetal alcohol spectrum disorders. Am J Med Genet C. 2004;127C:42-50.
- CDC. Alcohol use in pregnant and non-pregnant women of childbearing age – United States, 1991-2005. MMWR. 2010; 58(19):529-532.
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289(1):70-75.
- Tsai J, Floyd RL, Bertrand J. Tracking binge drinking among U.S. childbearing-age women. Preventive Medicine. 2007b;44:298-302.
- NIAAA. Binge drinking defined. Newsletter, Winter 2004, Number 3. National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. Rockville, Maryland: U.S. Department of Health and Human Services.
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38(2):90-96.
- Ebrahim SH, Diekman ST, Decoufle P, Tully M, Floyd RF. Pregnancy-related alcohol use among women in the United States, 1988-95. Prenatal Neonat Med. 1999;4:39-46.
- Ebrahim SH, Diekman ST, Floyd RL, Decoufle P. Comparison of binge drinking among pregnant and non-pregnant women, United States, 1991-1995. Am J Obstet Gynecol 1999;180:1-7.
- Kesmodel U. Binge drinking in pregnancy- frequency and methodology. American Journal of Epidemiology. 2001;154(8):777-782.
- Tough S, Tofflemire K, Clarke M, Newburn-Cook C. Do women change their drinking behaviors while trying to conceive? An opportunity for preconception counseling. Clinical Medicine & Research. 2006;4(2):97-105.
- Glik D, Prelip M, Myerson A, & Eilers K. Fetal alcohol syndrome prevention using community-based narrowcasting campaigns. Health Promotion Practice. 2008; 9(1):93-103.
- U.S. Department of Health and Human Services. Advisory on alcohol use in pregnancy; Feb 2005 Disponible sur le site: http://www.surgeongeneral.gov/pressreleases/sg02222005.html. Consulté le 1er août 2011.
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, December 2010.
- Guidelines for perinatal care. 5th ed. Elk Grove Village (IL): American Academy of Pediatrics; Washington, DC: American College of Obstetricians and Gynecologists; 2002.
- U.S. Department of Health and Human Services. Helping patients who drink too much: A clinician’s guide. Updated 2005 edition. NIH Publication No. 07-3769. Revised January 2007.
- Floyd RL, Decoufle P, Hungerford DW. Alcohol use prior to pregnancy recognition. Am J Prev Med. 1999;17(2): 101-107.
- U.S. Preventive Services Task Force. .Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med 2004;140:554-6.
- Chang et al. Brief interventions for prenatal alcohol use: a randomized trial. Obstetrics & Gynecology.2005; 105:991-8.
- O’Connor M, Whaley SE. Brief intervention for alcohol use by pregnant women. AJPH. 2007;97(2): 252-8.
- Floyd RL, Sobell M, Valesquez M, et al. Preventing alcohol-exposed pregnancies: a randomized controlled trial. Am J Prev Med. 2007;32(1):1-10.
- Barry KL, Caetano R, Chang G, DeJoseph MC, Miller LA, O’Connor MJ, Olson HC, Floyd RL, Weber MK, DeStefano F, Dolina S, Leeks K, National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Syndrome and Fetal Alcohol Effect. Reducing alcohol-exposed pregnancies: A report of the National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect. Atlanta, GA: Centers for Disease Control and Prevention: December 2008.
- Stade BC, Bailey C, Dzendoletas D, Sgro M, Dowswell T, Bennetttt D. Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy. Cochrane Database of Systematic Reviews. 2009, Issue 2. Art. No.:CD004228.DOI:10.1002/14651858.CD004228.pub2.
- Elek E., Harris S., Squire C., Margolis M. Formative focus groups on alcohol consumptions during pregnancy: Executive Summary. (2010) Unpublished report to CDC.
- Thomas JD, Warren KR, Hewitt BG. Fetal alcohol Spectrum Disorders – From research to policy. Alcohol Research & Health. 2010;33(1 and 2):118-126.
How to cite this article:
Floyd RL, Denny C, Weber MK. Prevention of Fetal Alcohol Spectrum Disorders. In: Tremblay RE, Boivin M, Peters RDeV, eds. O’Connor MJ, topic ed. Encyclopedia on Early Childhood Development [online]. https://www.child-encyclopedia.com/fetal-alcohol-spectrum-disorders-fasd/according-experts/prevention-fetal-alcohol-spectrum-disorders. Published: August 2011. Accessed January 13, 2026.
Text copied to the clipboard ✓