Obesity Prevention During Infancy: A Change of Focus
1Ian M. Paul, MD, MSc, 2Jennifer S. Savage, PhD, 2Stephanie Anzman-Frasca, PhD, 2Leann L. Birch, PhD
1Penn State College of Medicine, USA, 2Center for Childhood Obesity Research, Penn State University, USA
Introduction
Over the course of human history, feeding practices for newborns and infants have focused on ensuring adequate caloric intake to support adequate growth. These parenting practices evolved due to the possibility that famine was a common risk, and have persisted despite the unlikely occurrence of food scarcity in most of the developed world. Healthcare providers also have focused on ensuring adequate newborn and infant growth, and more specifically avoiding insufficient growth during the neonatal period and infancy, consistently guarding against the possibility of the diagnosis of “failure to thrive.” This however is problematic given that today, in the developed world, food is plentiful, and it is easy to obtain inexpensive, palatable, high-calorie foods even for very young children. Failure to thrive due to too few calories is uncommon, but parenting practices such as encouraging infants to finish bottles, “topping a child off” with extra calories before bedtime, pressuring infants to eat large servings of solid foods, and using food to soothe non-hunger related infant distress have persisted1 and can result in excessive weight gain during infancy. Healthcare providers also contribute to this problem from the first days of a baby’s life. While giving appropriate guidance to wake newborns every 3-4 hours to feed in the week following birth to prevent excessive neonatal weight loss, clinicians commonly neglect to inform parents to stop this practice once a baby returns to their birth weight and has established a healthy pattern of weight gain. Although most infants return to birth weight by age 2 weeks, a popular reference from the American Academy of Pediatrics recommends waking a baby that sleeps longer than 4-5 hours for a feeding during the first month.2 Further, clinicians continue to guard against failure to thrive but despite increasing rates of obesity, are very unlikely to diagnose excessive weight gain or obesity during infancy.3
Subject
In recent decades the prevalence of obesity has increased dramatically among all age groups, including infants and young children.4,5 Almost 10% of U.S. children less than 2 years are already obese and over 25% of children between ages 2 and 5 years are overweight.5 Across the globe, similar trends exist.6 Both overweight and rapid growth during infancy have significant long-term consequences, and are associated with adult obesity and its co-morbidities including hypertension, coronary artery disease and type 2 diabetes mellitus.7-10
Problems
Because infancy is a critical period of developmental plasticity with long-lasting metabolic and behavioural consequences,10,11 interventions developed for delivery during this period may alter long-term risk for obesity and associated co-morbidities. However, while modifiable factors promoting overweight and rapid growth during infancy have been identified,12-14 preventive interventions addressing these factors are scant.15 Further, both parents and healthcare providers must be educated to change their traditional focus from ensuring sufficient growth to recognizing and intervening upon early life obesity and its risk-factors.16,17
Research Context
Although it is a major public health problem with long-term consequences, parents and healthcare providers typically do not see early life obesity or rapid infant weight gain as problematic and instead often consider a chubby baby to be a healthy baby.18
Key Research Questions
Can the increasing prevalence of early life obesity be reversed?
Given the complex biological, behavioural and socioeconomic factors that interact to result in childhood obesity, what time periods in development should be targeted on both individual and societal levels and what are the most effective intervention components?
- What model is best for delivering obesity prevention interventions for infants (e.g., primary care-based, home visitation, other)?
- Can early life metabolic and behavioural influences on obesity be permanently changed via early life interventions?
- Is pregnancy or infancy the best time to intervene to prevent childhood obesity and its co-morbidities? Could interventions during both periods be synergistic?
Recent Research Results
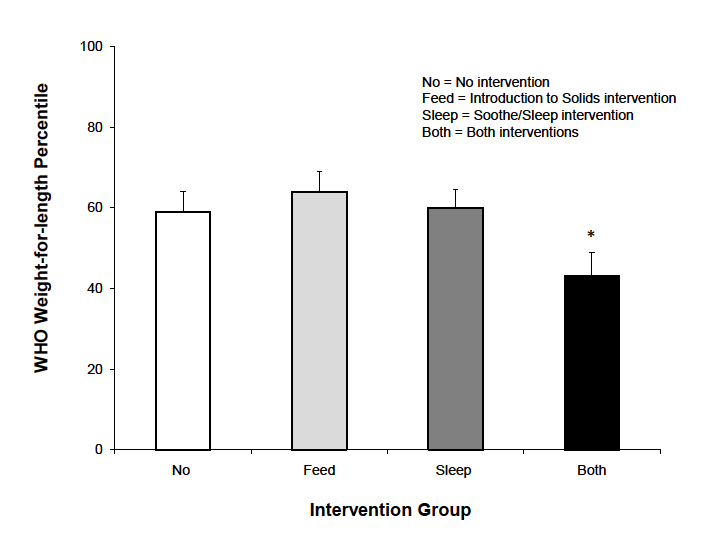
Prior to 2010, there were no intervention studies demonstrating beneficial effects on weight status of children younger than 2 years.19 Since then, two pilot studies showed positive effects on weight status of early intervention programs,20 and other trials are in progress.21-24 In one pilot, nurses assisted mothers in developing parenting skills related to three areas of infant behaviour believed to affect early obesity risk: sleeping, crying and feeding. First-time mothers who intended to breastfeed were randomly assigned to receive a soothe/sleep intervention, an introduction of solids intervention, both interventions, or no interventions. Interventions were delivered via home visits at ages 2-3 weeks and 4-6 months. One hundred and ten mother-infant pairs completed the one- year study. The soothe/sleep intervention focused on strategies to lengthen infant sleep and taught parents soothing strategies to use rather than indiscriminately feeding in response to infant fussing. At age 2-3 weeks, dyads randomized to this intervention were instructed on alternate soothing responses, including swaddling, side or stomach position, shushing, swinging, and (non-nutritive) sucking. Parents were also taught to emphasize day/night differences. The introduction of solids intervention focused on “when,” “how,” and “which” foods to introduce to infants and provided systematic experiences with new foods between ages 4-6 months. Infants receiving both interventions had significantly lower weight-for-length percentiles at 1 year compared to other groups. This result is depicted in Figure 1, where the y-axis depicts weight-for-length percentiles using the World Health Organization (WHO) growth charts.25
The second pilot study assessed a primary care based intervention to promote healthful behaviours among 0-6 month old infants and their mothers including motivational counseling and group parenting workshops.26 Eighty infants completed the 6-month trial with fewer intervention infants being in the highest quartile of weight-for-length z-score at 6 months of age (22% vs. 42%).
Research Gaps
While these pilot intervention results are promising, there are additional possible targets for the primary prevention of early life obesity27 including improving dietary content, increasing physical activity, reducing sedentary behaviours, improving sleep hygiene, improving parental understanding of normal infant growth, and improving parental responsiveness to infant cues and infant distress. For most candidate interventions, however, there are insufficient data on their effectiveness or data to support their reproducibility in and generalizability to different setting, cultures, or populations. Further, there is no evidence that early life prevention of overweight or obesity will lead to long-term prevention of obesity or its co-morbidities.
Conclusions
With obesity rates climbing for infants and toddlers globally, interventions are needed for this age group, given the lifelong consequences of early life obesity. Despite the limited evidence to date supporting interventions for obesity prevention during infancy, there has been increasing interest in this topic because infancy is a time of exceptional metabolic and behavioural plasticity. While there are numerous opportunities for intervention, a culture change among parents and pediatric healthcare providers is needed in order to change the primary focus of weight status in infancy from prevention of failure to thrive to the prevention of over-thriving. Societal acknowledgement of this problem and a change in focus by clinicians and parents will be timely as solutions appear to be forthcoming. In the meantime, those interested in the complexity of this topic plus potential solutions can review the Institute of Medicine’s recent publication, Early Childhood Obesity Prevention Policies, which focuses on the period from birth to age 5 and includes brief reviews of the evidence for some of these factors influencing early growth in infancy and early childhood.18
Implications for Parents, Services and Policy
In our current obesogenic environment, it has become easier for parents, healthcare providers, and policy makers to view being overweight as normal. Unfortunately, obesity and its co-morbidities may have devastating health effects for individuals and economic effects on a societal level. Failure to recognize overweight infants is common and its consequences can be dire. Fortunately, research into promising interventions is increasing, and policy makers are drawing attention to the problem. First Lady Michelle Obama’s program, “Let’s Move,” aims to solve the childhood obesity epidemic within a generation and includes messages that begin during pregnancy and infancy, such as the promotion of breastfeeding as the preferred source for infant nutrition.28 In addition, the recent Institute of Medicine report on Early Childhood Obesity Prevention Policies focuses on preventing obesity during infancy and early childhood.18 Policy recommendations include promoting growth monitoring and early screening by healthcare professionals to identify infants and young children who may be at risk based on early growth. The report also includes policies designed to impact developing lifestyle behaviours associated with increased obesity risk, including sleep, eating patterns, physical activity and media exposure. The recommendations are based on current evidence and the evidence-based belief that changing policy can change obesity. The report also highlights the need for research to evaluate the impact of policy recommendations and to develop more effective early interventions. All of these programs and research demonstrate clearly that our society must shift its traditional primary focus from ensuring adequate growth to the preventing obesity.
Figure 1. Infants who received both interventions had lower weight-for-length percentiles at age 1 year (n=110), relative to the WHO growth standards. (Adapted from Paul et al. Preventing Obesity during Infancy: A Pilot Study. Obesity 2011; 19: 353-6120).
References
- Black MM, Siegel EH, Abel Y, Bentley ME. Home and videotape intervention delays early complementary feeding among adolescent mothers. Pediatrics 2001;107:E67.
- Shelov SP, Hannemann RE, eds. Caring for your baby and young child: Birth to age 5. 5th ed: Bantam Books; 2009.
- McCormick DP, Sarpong K, Jordan L, Ray LA, Jain S. Infant obesity: are we ready to make this diagnosis? J Pediatr 2010;157:15-9.
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA 2002;288:1728-32.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 2012;307:483-90.
- de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr;92:1257-64.
- Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med 1993;22:167-77.
- Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 2002;109:194-9.
- Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA 2009;301:2234-42.
- Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 2008;359:61-73.
- Gluckman PD, Hanson MA. Developmental and epigenetic pathways to obesity: an evolutionary-developmental perspective. Int J Obes (Lond) 2008;32 Suppl 7:S62-71.
- Paul IM, Bartok CJ, Downs DS, Stifter CA, Ventura AK, Birch LL. Opportunities for the Primary Prevention of Obesity during Infancy. Adv Pediatr 2009;56:107-33.
- Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW, Taveras EM. Developmental origins of childhood overweight: potential public health impact. Obesity (Silver Spring) 2008;16:1651-6.
- Anderson SE, Whitaker RC. Household Routines and Obesity in US Preschool-Aged Children. Pediatrics 2010;125:420-8.
- Hesketh KD, Campbell KJ. Interventions to Prevent Obesity in 0-5 Year Olds: An Updated Systematic Review of the Literature. Obesity (Silver Spring) 2010;18:S27-S35.
- Laraway KA, Birch LL, Shaffer ML, Paul IM. Parent perception of healthy infant and toddler growth. Clin Pediatr (Phila) 2010;49:343-9.
- Sullivan SA, Leite KR, Shaffer ML, Birch LL, Paul IM. Urban parents' perceptions of healthy infant growth. Clin Pediatr (Phila);50:698-703.
- Birch LL, Parker L, Burns A, eds. Early Childhood Obesity Prevention. Washington, D.C.: Institute of Medicine; 2011.
- Ciampa PJ, Kumar D, Barkin SL, et al. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Arch Pediatr Adolesc Med;164:1098-104.
- Paul IM, Savage JS, Anzman SL, et al. Preventing obesity during infancy: a pilot study. Obesity (Silver Spring) 2011;19:353-61.
- Wen LM, Baur LA, Rissel C, Wardle K, Alperstein G, Simpson JM. Early intervention of multiple home visits to prevent childhood obesity in a disadvantaged population: a home-based randomised controlled trial (Healthy Beginnings Trial). BMC Public Health 2007;7:76.
- Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster-randomised controlled trial. BMC Public Health 2008;8:103.
- Wen LM, Baur LA, Rissel C, et al. Healthy Beginnings Trial Phase 2 study: Follow-up and cost-effectiveness analysis. Contemp Clin Trials 2011.
- Daniels LA, Magarey A, Battistutta D, et al. The NOURISH randomised control trial: positive feeding practices and food preferences in early childhood - a primary prevention program for childhood obesity. BMC Public Health 2009;9:387.
- Grummer-Strawn LM, Reinold C, Krebs NF. Use of World Health Organization and CDC growth charts for children aged 0-59 months in the United States. MMWR Recomm Rep 2010;59:1-15.
- Taveras EM, Blackburn K, Gillman MW, et al. First steps for mommy and me: a pilot intervention to improve nutrition and physical activity behaviors of postpartum mothers and their infants. Matern Child Health J 2010;15:1217-27.
- Paul IM, Bartok CJ, Downs DS, Stifter CA, Ventura AK, Birch LL. Opportunities for the primary prevention of obesity during infancy. Adv Pediatr 2009;56:107-33.
- Wojcicki JM, Heyman MB. Let's Move--childhood obesity prevention from pregnancy and infancy onward. N Engl J Med 2010;362:1457-9.
How to cite this article:
Paul IM, Savage JS, Anzman-Frasca S, Birch LL. Obesity Prevention During Infancy: A Change of Focus. In: Tremblay RE, Boivin M, Peters RDeV, eds. Fisher JO, topic ed. Encyclopedia on Early Childhood Development [online]. https://www.child-encyclopedia.com/child-obesity/according-experts/obesity-prevention-during-infancy-change-focus. Published: April 2012. Accessed February 27, 2026.
Text copied to the clipboard ✓