Clinical Assessment of Individuals with Fetal Alcohol Spectrum Disorders (FASD)
Susan Astley, PhD
Washington State Fetal Alcohol Syndrome Diagnostic & Prevention Network (FASDPN), USA
Introduction
Fetal Alcohol Syndrome (FAS) is a permanent birth defect syndrome caused by maternal consumption of alcohol during pregnancy. The condition is characterized by growth deficiency, a unique cluster of minor facial anomalies and central nervous system (CNS) abnormalities.1 The prevalence of FAS is estimated to be 1-3/1,000 live-births1 in the general population, and as high as 10-15/1,000 in high-risk populations like foster care.2 Not all individuals exposed and damaged by alcohol have FAS. Most present neuropsychological impairments without the physical findings. The condition is now recognized as a spectrum of disorders, FASD. Diagnoses like FAS, Partial FAS (PFAS), Alcohol-Related Neurodevelopmental Disorder (ARND), Static Encephalopathy/Alcohol -Exposed (SE/AE) and Neurobehavioural Disorder/Alcohol-Exposed (ND/AE) fall under the umbrella of FASD.1,3
Subject
Although reference to the harmful effects of maternal drinking on infant outcome date back to biblical times,4,5,6 the term FAS was not coined until 1973.7-9,10,11 Diagnostic guidelines were developed and refined through the 70s and 80s,7,12,13,14 culminating in 1996 with the publication of the Institute of Medicine (IOM) guidelines.1 While the IOM guidelines reflected an important advancement, the IOM committee continued to feel: 1) “a medical diagnosis of FAS remained the purview of dysmorphologists and clinical geneticists,” and 2) the guidelines remained intentionally broad and conceptual (gestalt) rather than specific and operational (case-defined).15,16 For example, the guidelines for CNS dysfunction did not address how many areas of deficit must be present or how severe the deficits must be. The guidelines for the facial phenotype did not address how many features must be present, how severe each feature must be, or what measurement scales should be used to judge their severity. And introduction of the term ARND ran counter to the retraction of the term Fetal Alcohol Effects (FAE) the year prior.17 Overall, guidelines through 1996 were not sufficiently specific to ensure diagnostic accuracy (the ability to derive the correct diagnosis) or diagnostic reproducibility (the ability for two different clinicians to derive the same diagnosis in a given patient).18
Problems
In the absence of an accurate/reproducible method of diagnosis, diagnoses continued to vary widely between clinics.1,18,19 From a clinical perspective, diagnostic misclassification leads to inappropriate patient care, increased risk for secondary disabilities20 and missed opportunities for prevention.15,21,22 From a public health perspective, diagnostic misclassification leads to inaccurate prevalence estimates.15 Inaccurate estimates thwart efforts to allocate sufficient social/educational/medical services to this high-risk population and preclude the accurate assessment of prevention efforts. From a research perspective, diagnostic misclassification prevents detection of clinically-meaningful contrasts between groups and valid comparisons of outcomes between studies.23
Research Context
To overcome the limitations of the physician-focused gestalt approach to FASD diagnosis, the FASDPN introduced an interdisciplinary team approach in 1993 (medical doctor, psychologist, speech-language pathologist and occupational therapist)24,25 guided by a rigorous, case-defined set of guidelines (FASD 4-Digit Diagnostic Code) in 1997.15,16 Briefly, the 4 digits of the 4-Digit Code reflect the magnitude of expression of the 4 key diagnostic features of FASD in the following order: 1) growth deficiency, 2) FAS facial phenotype, 3) CNS structural/functional abnormalities, and 4) prenatal alcohol exposure (Fig. 1).15 The magnitude of expression of each feature is ranked on a 4-point scale, with 1 reflecting complete absence of the feature and 4 reflecting severe presence of the feature. Each rank is specifically case-defined. The 4-Digit codes range from 1111 to 4444. To date, every combination of Code has been observed in the FASDPN clinics, reflecting the true diversity of outcome associated with prenatal alcohol exposure. The subset of 4-Digit Codes that fall under the umbrella of FASD can be grouped into three clinically meaningful and distinct diagnostic subgroups:
- FAS/PFAS (severe neuropsychological impairment with the FAS facial phenotype);
- SE/AE (severe neuropsychological impairment without the facial phenotype); and
- ND/AE (moderate neuropsychological impairment without the facial phenotype).23,26,27
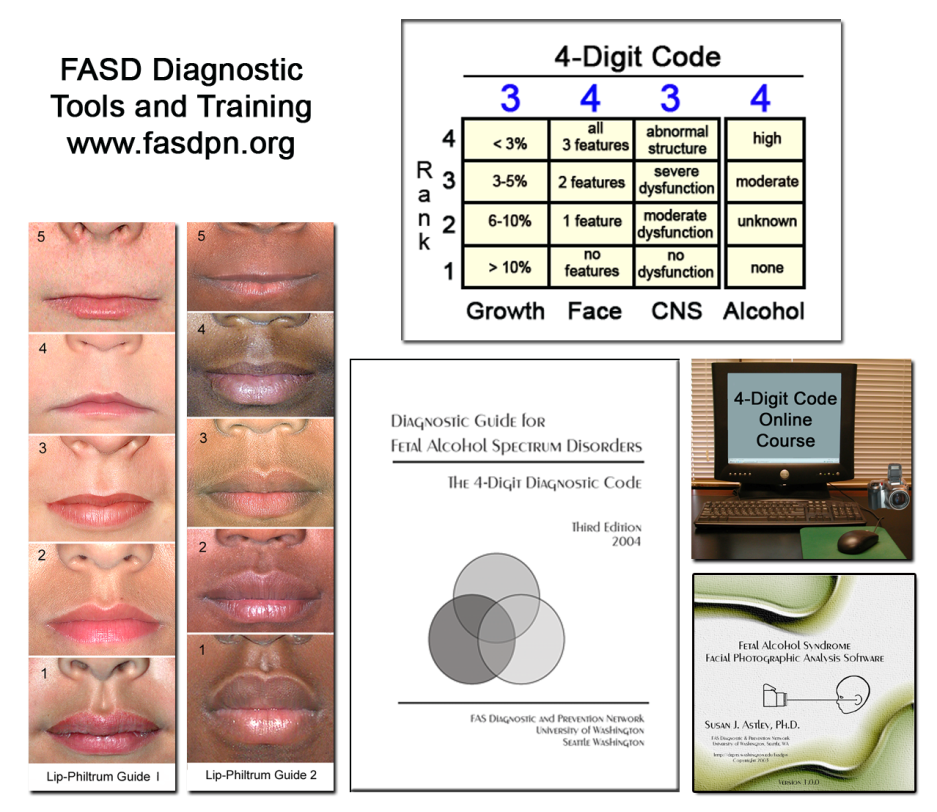
Figure 1. Fetal Alcohol Spectrum Disorders: 4-Digit Diagnostic Code: guide, tools and training.
Key Research Questions
Requisite to the development of diagnostic guidelines is validation of their performance, both before and after their release. Performance should be authenticated through published empirical studies. Measures of performance include accuracy, reproducibility, validity, and practicality.28 Diagnostic teams should look for the following benchmarks in current FASD diagnostic guidelines:1,3,28-32
- Are the guidelines evidence-based and developed from a broad, representative population-base? The evidence-base should include validation of performance prior to the guideline’s release.
- Do the guidelines endorse an interdisciplinary approach to diagnosis?
- Are the diagnostic criteria specifically and comprehensively case-defined?
- Do the diagnostic tools maximize measurement accuracy and precision?
- The features that characterize FASD (growth, face, CNS, alcohol) are not simply present or absent. Each present along separate, clinically meaningful continua. Are these continua reflected in the guideline’s measurement and classification scales?
- The validity of an FAS diagnosis rests entirely on its unique facial phenotype. Therefore, the sensitivity and specificity of the FAS facial phenotype must be high (>90%) and empirically confirmed. Do the guideline’s facial criteria meet these criteria?
- Do the guidelines identify diagnostic subgroups that are: a) clinically and statistically distinct from one another, b) reflect a continuum of increasing neuropsychological and physical abnormality, and c) span the full continuum of FASD?
- Does the diagnostic nomenclature assert clinical integrity?
- The validity of the scales used to measure and classify exposures and outcomes is demonstrated by their ability to detect statistically-significant, physiologically meaningful correlations between physical outcomes, functional outcomes and alcohol exposure levels. With the scales: Does face predict brain? Does neurofunction correlate with neurostructure? Do diagnostic subgroups have unique alcohol-exposure patterns?
- Are the guidelines readily adoptable into clinical practice? Their practicality should not be at the expense of their accuracy and precision. Training should be expedient, affordable, universally available and competency-based.
Recent Research Results
Below are examples of how the FASD 4-Digit Code meets all 10 benchmarks.
- Evidence-based: The medical records of 1,014 patients (newborn-adult, all races) receiving FASD diagnostic evaluations in the statewide FASDPN were used to develop the 4-Digit Code. Its performance was validated prior to its release through both empirical analysis and a two-year trial of use by an interdisciplinary team.15
- Interdisciplinary approach: The guidelines necessitate the measurement and differential interpretation of physical (growth and dysmorphology) and functional (psychological, language, motor-sensory) outcomes, often in the context of complex social/environmental settings. This requires the expertise of an interdisciplinary team.25,26
- Case-definitions, measurement tools: Continuum of exposure and outcome: Case-definitions, measurement tools: All criteria are specifically/operationally case-defined. For example, in contrast to the IOM definition of the FAS facial phenotype (“a characteristic pattern that includes features such as short palpebral fissure length (PFL), flat upper lip, flattened philtrum and flat midface”),1 the 4-Digit Code defines how short, how thin, and how smooth these first three features must be, and provides tools (Lip-Philtrum Guides and FAS Facial Photographic Analysis Software33) to accurately measure these features along their full continuum. The 4-Digit Code also recognizes the FAS facial phenotype is not simply present or absent. Its magnitude of expression is measured on a 4-point scale.15
- Continuum of exposure and outcome: All FASD features are measured and classified on continuous or ordinal scales. Lips and philtrums are measured on 5-point Likert scales. Growth, face, CNS and alcohol are ranked on 4-point scales (Fig. 1). Even the diagnostic subgroups (ND/AE, SE/AE, and FAS/PFAS) reflect three distinct groups with increasing physical/functional impairment.15,23,26,27,34,35
- Specificity of FAS face: The Rank 4 FAS facial phenotype is over 95% sensitive and specific to FAS and prenatal alcohol exposure.2,36,37
- Distinct diagnostic subgroups: MRI /MRS /fMRI 23,26,27,34,35 have confirmed ND/AE, SE/AE and FAS/PFAS are three clinically distinct, increasingly more severe diagnostic subgroups with unique alcohol exposure patterns. For example, although FAS/PFAS and SE/AE both present with severe dysfunction and disproportionately smaller caudates, only FAS/PFAS has the full FAS facial phenotype, disproportionately smaller frontal lobes, significantly lower neurocholine levels, and a significantly higher frequency and duration of alcohol exposure. And although neither SE/AE nor ND/AE present with the full FAS facial phenotype, SE/AE presents with more severe dysfunction, disproportionately smaller caudates and a significantly higher quantity of alcohol exposure. And despite ND/AE’s moderate dysfunction, MRI confirms a high prevalence of underlying neurostructural abnormality.
- Nomenclature integrity: The terms SE/AE and ND/AE replace the terms ARND and FAE to accurately document an individual’s outcomes and exposure without implying a causal association has been confirmed (or ruled-out) between the two.15,17,28,29
- Validity: Published empirical studies2,15,23,26,27,34-37 document a broad array of physiologically cogent relationships between exposures and outcomes. A few examples: Face predicts brain: IQ and regional brain volumes decrease incrementally and significantly with increasing expression (Ranks 1-4) of the FAS facial phenotype. Neurofunction correlates with neurostructure: The 3-point scale for CNS dysfunction (Rank 1=none, Rank 2=moderate, Rank 3=severe) is significantly associated with decreasing caudate volume.
- Readily adoptable into practice: The guidelines and tools are distributed free or at cost via the web. Training is online, accredited, low-cost and can be completed in a weekend.38
Research Gaps
The problems (outlined above) that initially hindered FASD diagnosis have now been overcome with the adoption of rigorous diagnostic guidelines administered by interdisciplinary teams.2,3,15,23,26-28,34,35,37,39 It is now time to focus research on FASD intervention.40
Conclusions
The FASD 4-Digit Diagnostic Code offers an intuitively logical, numeric approach to reporting outcomes and exposure that reflects the true diversity and continuum of disability associated with prenatal alcohol exposure. It also offers substantially greater precision, accuracy and validity than the gestalt method of diagnosis, through the use of quantitative measurement scales, specific case-definitions and an interdisciplinary team approach.
Implications for Parents, Services and Policy
Parents (830 over 13 years) have expressed high satisfaction with the FASDPN interdisciplinary approach to diagnosis using the 4-Digit Code.26 They report the method was easy to understand and provided them with information they were unable to obtain elsewhere (99% would recommend the clinic to others). The FASDPN model has also earned the respect of service providers statewide. The diagnostic reports provide the detail and direction providers need to qualify children for services. Parents of children with FAS/PFAS, SE/AE and ND/AE confirm being able to access and benefit from recommended interventions.26 The interdisciplinary model and 4-Digit Code have been adopted worldwide, often initiated and supported through legislative policy.26,41-44
References
- Stratton KR, Howe CJ, Battaglia FC, eds. Fetal alcohol syndrome: Diagnosis, epidemiology, prevention, and treatment. Washington, DC: National Academy Press; 1996.
- Astley S, Stachowiak J, Clarren S, Clausen C. Application of the fetal alcohol syndrome facial photographic screening tool in a foster care population. Journal of Pediatrics 2002;141(5):712-7.
- Astley SJ. Diagnostic guide for fetal alcohol spectrum disorders: The 4-Digit Diagnostic Code. 3rd ed. Seattle, WA: University of Washington Publication Services; 2004.
- Goodacre K. Guide to the Middlesex Sessions Records 1549–1889. London, UK: Greater London Record Office, Middlesex Records; 1965.
- Royal College of Physicians of London. Royal College of Physicians of London annals. London, UK; 1726.
- Sullivan W. A note on the influence of maternal inebriety on the offspring. Journal Mental Science 1899;45:489-503.
- Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet 1973;2(7836):999-1001.
- Jones K, Smith D, Ulleland C, Streissguth A. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet 1973;1:1267-71.
- Lemoine P, Harousseau H, Borteyni J, Menuet J. Les enfants de parents alcooliques: anomalies observées. A propos de 127 cas [The children of alcoholic parents: anomalies observed in 127 cases]. Quest Medicale 1968;8:476-82.
- Ulleland C. The offspring of alcoholic mothers. Annals New York Academy of Sciences 1972;197:167-9.
- Ulleland C, Wennberg R, Igo R, Smith N, eds. The offspring of alcoholic mothers. Jersey City, NJ: American Pediatric Society and Society for Pediatric Research; 1970.
- Clarren SK, Smith DW. The fetal alcohol syndrome. New England Journal of Medicine 1978;298(19):1063-1067.
- Rosett HL. A clinical perspective of the fetal alcohol syndrome. Alcoholism: Clinical and Experimental Research 1980;4(2):199-122.
- Sokol RJ, Clarren SK. Guidelines for use of terminology describing the impact of prenatal alcohol on the offspring. Alcoholism: Clinical and Experimental Research 1989;13(4)597-598.
- Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: introducing the 4-digit diagnostic code. Alcohol and Alcoholism 2000;35(4):400-410.
- Astley SJ, Clarren SK. Diagnostic guide for fetal alcohol syndrome and related conditions: The 4-digit diagnostic code. 1st ed. Seattle, WA: University of Washington Publication Services; 1997.
- Aase JM, Jones KL, Clarren SK. Do we need the term “FAE”? Pediatrics 1995;95(3):428-430.
- Aase JM. Clinical recognition of FAS: difficulties of detection and diagnosis. Alcohol Health and Research World 1994;18(1):5-9.
- Chavez GF, Cordero JF, Becerra JE. Leading major congenital malformations among minority groups in the United States, 1981-1986. Morbidity and Mortality Weekly Report. Surveillance summaries: MMWR / Centers for Disease Control 1988;37(SS-03):17-24.
- Streissguth AP, Kanton J, eds. The challenge of fetal alcohol syndrome: Overcoming secondary disabilities. Seattle, WA: University of Washington Press; 1997.
- Astley SJ, Bailey D, Talbot T, Clarren SK. Fetal alcohol syndrome (FAS) primary prevention through FAS diagnosis: I. Identification of high-risk birth mothers through the diagnosis of their children. Alcohol & Alcoholism 2000;35(5):499-508.
- Astley SJ, Bailey D, Talbot T, Clarren SK. Fetal alcohol syndrome (FAS) primary prevention through FAS diagnosis: II. A comprehensive profile of 80 birth mothers of children with FAS. Alcohol & Alcoholism 2000;35(5):509-519.
- Astley SJ, Aylward EH, Olson HC, Kerns K, Brooks A, Coggins TE, Davies J, Dorn S, Gendler B, Jirikowic T, Kraegel P, Maravilla K, Richards T. Magnetic resonance imaging outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. Alcohol: Clinical and Experimental Research 2009;33(10):1-19.
- Clarren SK, Astley SJ. Development of the FAS diagnostic and prevention network in Washington State. In: Streissguth AP, Kanton J, eds. The challenge of fetal alcohol syndrome: Overcoming secondary disabilities. Seattle, WA: University of Washington Press; 1997:40-51.
- Clarren SK, Carmichael Olson H, Clarren SGB, Astley SJ. A child with fetal alcohol syndrome. In: Guralnick MJ, ed. Interdisciplinary clinical assessment of young children with developmental disabilities. Baltimore, MD: Paul H. Brookes Publishing Co; 2000: 307-326.
- Astley SJ. Profile of the first 1,400 patients receiving diagnostic evaluations for fetal alcohol spectrum disorder at the Washington State Fetal Alcohol Syndrome Diagnostic & Prevention Network. Canadian Journal of Clinical Pharmacology 2010;17(1):e132-64.
- Astley SJ, Olson HC, Kerns K, Brooks A, Aylward EH, Coggins TE, Davies J, Dorn S, Gendler B, Jirikowic T, Kraegel P, Maravilla K, Richards T. Neuropsychological and behavioral outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. Canadian Journal of Clinical Pharmacology. 2009;16(1):e178-e201.
- Astley SJ. Diagnosing fetal alcohol spectrum disorders. In: Adubato S, Cohen D, eds. Prenatal alcohol use and fetal alcohol spectrum disorders: Historical and future perspectives. Oak Park, IL: Bentham Publishers. In press.
- Astley SJ. Comparison of the 4-digit diagnostic code and the hoyme diagnostic guidelines for fetal alcohol spectrum disorders. Pediatric Review 2006;118(4):1532-45.
- Bertrand J, Floyd RL, Weber MK, O’Connor M, Riley EP, Johnson KA, Cohen E, eds. Fetal alcohol syndrome: Guidelines for referral and diagnosis. Atlanta, GA: Centers for Disease Control and Prevention; 2004.
- Chudley AE, Conroy J, Cook JL, Loock C, Rosales T, LeBlanc N, Public Health Agency of Canada’s National Advisory Committee on Fetal Alcohol Spectrum Disorder. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Canadian Medical Association Journal 2005;172:S1-S21.
- Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, Buckley DG, Miller JH, Aragon AS, Khaole N, Viljoen DL, Jones KL, Robinson LK. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 Institute of Medicine criteria. Pediatrics 2005;115:39-47.
- Astley SJ. Fetal alcohol syndrome facial photograph analysis software. Version 1.0. Seattle, WA: University of Washington; 2003.
- Astley SJ, Aylward EH, Olson HC, Kerns K, Brooks A, Coggins TE, Davies J, Dorn S, Gendler B, Jirikowic T, Kraegel P, Maravilla K, Richards T. Functional magnetic resonance imaging outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. Journal of Neurodevelopmental Disorders 2009;1(1):61-80.
- Astley SJ, Richards T, Aylward EH, Olson HC, Kerns K, Brooks A, Coggins T, Davies J, Dorn S, Gendler B, Jirikowic T, Kraegel P, Maravilla K. Magnetic resonance spectroscopy outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. Magnetic Resonance Imaging 2009;27:760-78.
- Astley SJ, Clarren SK. A case definition and photographic screening tool for the facial phenotype of fetal alcohol syndrome. Journal of Pediatrics 1996;129:33-41.
- Astley SJ, Clarren SK. Measuring the facial phenotype of individuals with prenatal alcohol exposure: correlations with brain dysfunction. Alcohol and Alcoholism 2001;36(2):147-159.
- Astley SJ. Online course: (2004) FASD 4-digit diagnostic code. Disponible sur le site: http://depts.washington.edu/fasdpn/htmls/online-train.htm. Accessed February 9, 2011.
- Astley SJ. Fetal alcohol syndrome prevention in Washington State: Evidence of success. Paediatric and Perinatal Epidemiology 2004;18:344-51.
- Bertrand J. Interventions for children with fetal alcohol spectrum disorders (FASDs): Overview of findings for five innovative research projects. Research in Developmental Disabilities 2009;30:986-1006.
- Mutch R, Peadon EM, Elliott EJ, Bower C. Need to establish a national diagnostic capacity for foetal alcohol spectrum disorders. Journal of Paediatric and Child Health 2009;45(3):79-81.
- New Jersey Task Force on Fetal Alcohol Disorders. The Governor’s Council on Prevention of Mental Retardation and Developmental Disabilities. Be in the kNOw: A 5-year strategic plan to prevent perinatal addictions in New Jersey. Trenton, NJ: The Governor’s Council on Prevention of Mental Retardation and Developmental Disabilities. New Jersey Task Force on Fetal Alcohol Disorders; 2007.
- State of Alaska. Department of Health and Social Services. Division of Behavioral Health. FASD diagnostic services provider agreement – AMENDED. Juneau, AK: Division of Behavioral Health. Department of Health and Social Services. State of Alaska. Form 06-5896 Provider Agreement (Rev6/05).
- State of Washington, Substitute Senate Bill 5688, Chapter 54, Laws of 1995, 54th Legislature, 1995 Regular Session, Fetal Alcohol Exposure Prevention, Effective Date: 7/23/95
How to cite this article:
Astley S. Clinical Assessment of Individuals with Fetal Alcohol Spectrum Disorders (FASD). In: Tremblay RE, Boivin M, Peters RDeV, eds. O’Connor MJ, topic ed. Encyclopedia on Early Childhood Development [online]. https://www.child-encyclopedia.com/fetal-alcohol-spectrum-disorders-fasd/according-experts/clinical-assessment-individuals-fetal. Published: February 2011. Accessed March 9, 2026.
Text copied to the clipboard ✓